 |
REFERENCES:
- Fernández, J. et al. Standard for collecting and reporting outcomes of IOL–based refractive surgery: update for enhanced monofocal, EDOF, and multifocal IOLs. J Cataract Refract Surg 48, 1235–1241 (2022).
-
Reinstein, D. Z. & Waring, G. O. Graphic Reporting of Outcomes of Refractive Surgery. J Refract Surg 25, 975–978 (2009).
 |
Software and Tools IncludedWith the course we provide you with the "Refractive Analysis" which is an easy to use software that has been built on basis of the Refractive Analysis Toolbox used in scientific studies in order to conduct common operations related to Anterior Segment Surgery or graphical representations according to the standards of peer review journals. Publications that have used the Refractive Analysis Toolbox have been classified by the Journal of Refractive Surgery as great examples of analysis. |
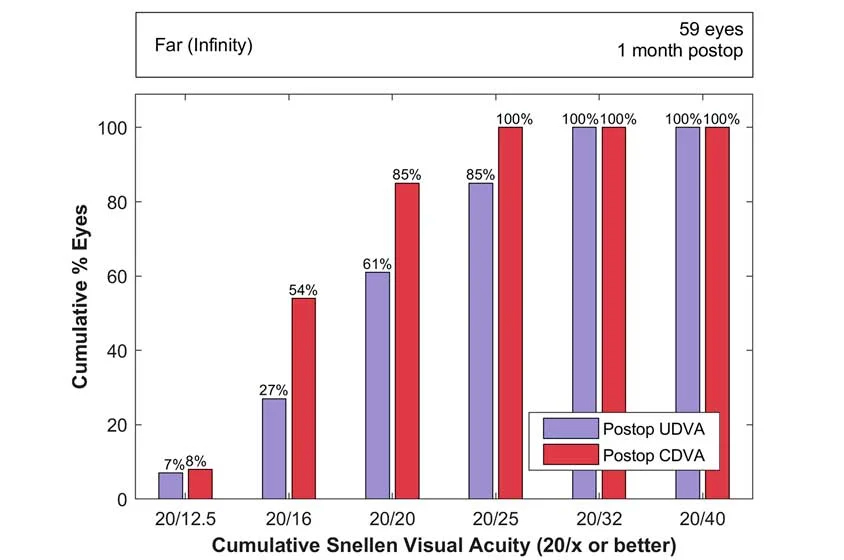
Standards EvolutionStandardization in refractive and cataract surgery reporting began in the early 90s, marking a shift from an era of no formalized standards. A series of charts was proposed to streamline the representation of surgical results. However, the initial proposals were not widely accepted until the late 90s. By 2000, a set of six standardized charts was established, promoting easier adoption by authors, clearer requirements by editors, and better understanding by readers. By 2009, the adoption of these standardized charts became mandatory in most research journals, prompting enhancements to improve precision and accuracy. In 2011, the standards were globally adopted and further extended to include specific terminologies. The evolution continued with the introduction of astigmatism results reporting standards in 2014, and a shift from single to double-angle charts in 2018 for better representation of astigmatism analysis. In 2017, separate standards for cataract surgery reporting were introduced, including specific guidelines for studies involving intraocular lens calculation formulas. These standards received further updates in 2021 and 2022 to cater for advancements in lens technology. The ongoing evolution underpins a commitment to improving clarity, accuracy, and comprehension in refractive and cataract surgery reporting. |
|
|
|
|